Diagnosis and Personalized Treatment of Inflammatory Bowel Disease
Update Date:2025/01/06,
Views:117
Dr. Zhang Zhao-Feng and Dr. Xie Ming-Jun from the Gastroenterology Division
What is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease (IBD) is a chronic and relapsing intestinal inflammatory condition, primarily consisting of two major types: Ulcerative Colitis (UC) and Crohn's Disease (CD). These diseases are autoimmune-related, where the immune system abnormally attacks the intestinal tissues. The clinical manifestations of IBD typically alternate between acute flare-ups and periods of remission, leading to chronic inflammation and the potential for complications.
Ulcerative Colitis mainly affects the mucosal layer of the colon and rectum, causing continuous ulcers and inflammation. Crohn's Disease, on the other hand, can affect any part of the digestive tract, from the mouth to the anus, and the inflammation can involve all layers of the intestinal wall. While the symptoms of both diseases are similar, the affected areas and the underlying mechanisms of the diseases differ, requiring accurate diagnosis for appropriate treatment.
Common Symptoms and High-Risk Groups
Main Symptoms:
1. Diarrhea: Chronic, recurrent diarrhea is the most common symptom, and stools may contain blood or mucus.
2. Abdominal Pain: Typically presents as recurrent pain in the lower abdomen or right lower abdomen, especially in patients with Crohn's Disease.
3. Rectal Bleeding: Blood in stools is more common in patients with Ulcerative Colitis.
4. Weight Loss and Fatigue: Due to prolonged malnutrition or chronic inflammation.
5. Fever: Often occurs during active disease phases; it is important to monitor for possible coexisting infections.
High-Risk Groups:
• Age: The disease most commonly affects individuals aged 20-40, but it can also occur in children and the elderly.
• Gender: Males are slightly more likely to be affected, especially in the case of Ulcerative Colitis.
• Genetic and Environmental Factors: A family history of IBD and modern dietary habits may increase the risk of developing the condition.
How to Diagnose Inflammatory Bowel Disease (IBD)?
The diagnosis of IBD requires a comprehensive approach, integrating clinical presentation, imaging studies, endoscopic examination, and laboratory tests. The following are common diagnostic methods:
1. Clinical History: Document the duration and frequency of symptoms, as well as the family medical history.
2. Blood and Stool Tests: These help confirm inflammation markers, such as elevated C-reactive protein (CRP), fecal occult blood, and fecal calprotectin.
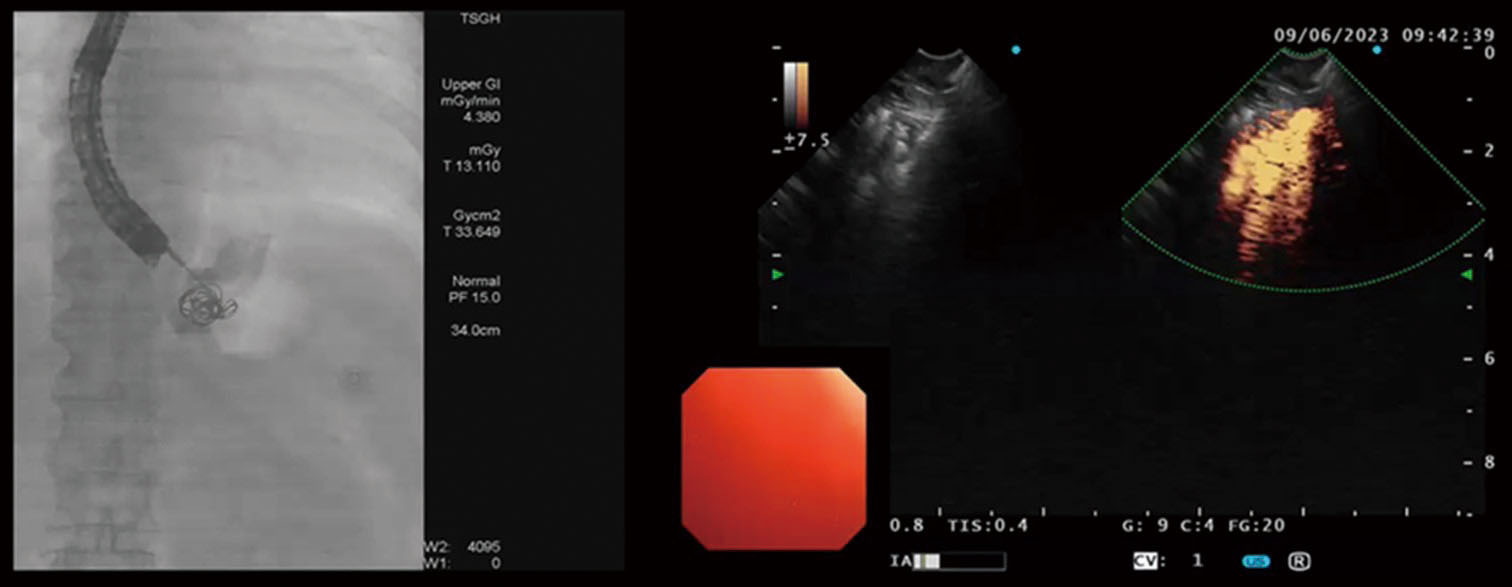
3. Endoscopic Examination: Colonoscopy and gastroscopy are key methods for confirming ulcers and obtaining biopsy samples.
4. Imaging Studies: Techniques like magnetic resonance imaging (MRI) enterography or computed tomography (CT) scans can examine the small intestine, often affected by Crohn's Disease.
5. Pathological Biopsy: Biopsy samples from intestinal tissue are analyzed to confirm the characteristic features of the disease.
The Importance of Personalized Treatment for Inflammatory Bowel Disease (IBD)
The primary goal in treating IBD is to reduce inflammation, alleviate symptoms, and prevent complications. Given the variation in patients' conditions, lifestyles, and genetic backgrounds, personalized treatment is crucial for improving overall quality of life. The following are common treatment approaches:
Medications:
1. Anti-inflammatory Drugs: Such as Budesonide or 5-Aminosalicylic Acid (5-ASA), used for mild to moderate cases.
2. Corticosteroids: Effective during acute flare-ups, but long-term use requires caution due to potential side effects.
3. Immunosuppressants: Medications like Azathioprine or Methotrexate, which help control immune responses.
4. Biologics: Tumor Necrosis Factor (TNF) inhibitors, specific cytokine inhibitors, or oral small molecule drugs, which represent breakthrough treatments for moderate to severe IBD.
Surgical Treatment: Surgery may be necessary if medication is ineffective or complications such as bowel perforation or strictures arise. Procedures may include colectomy or ostomy.
Dietary and Lifestyle Management:
• Avoid high-fat and processed foods, and increase the intake of low-fiber, easily digestible foods.
• Psychological support is emphasized, as stress can exacerbate the condition.
Latest Trends and Future Outlook
With advancements in genetic sequencing and microbiological research, the future of Inflammatory Bowel Disease (IBD) treatment will become more precise, with a greater emphasis on interdisciplinary healthcare teams. In addition to the traditional treatment options, personalized probiotics tailored to the patient's gut microbiome, fecal microbiota transplantation, and gene-assisted medication guidance are expected to further improve therapeutic outcomes.
In conclusion, IBD is a chronic disease that requires lifelong management. Patients and their families should work closely with healthcare teams to achieve the best quality of life for the patient.